INTERVENTIONAL CARDIOLOGY
IMAGE IN CARDIOVASCULAR MEDICINE
Cardiology Journal
2023, Vol. 30, No. 4, 673–674
DOI: 10.5603/cj.94722
Copyright © 2023 Via Medica
ISSN 1897–5593
eISSN 1898–018X
Successful percutaneous coronary intervention with rotational atherectomy in calcified lesion: Insight from optical coherence tomography
Seohong Min1Sungjin Kim1Hongjun Lee1Suyoung Lee1Yongcheol Kim2
1Severance Hospital, Seoul, Republic of Korea
2Division of Cardiology, Department of Internal Medicine, Yonsei University College of Medicine and Cardiovascular Center, Yongin Severance Hospital, Yongin, Republic of Korea
Address for correspondence: Yongcheol Kim, MD, PhD, FACC, FESC, FAPSC, Cardiovascular Center, Yongin Severance Hospital, 363 Dongbaekjukjeon-daero, Giheung-gu, Yongin 16995, Republic of Korea, e-mail: Yongcheol@yuhs.ac
Received: 19.03.2023 Accepted: 16.07.2023
This article is available in open access under Creative Common Attribution-Non-Commercial-No Derivatives 4.0 International (CC BY-NC-ND 4.0) license, allowing to download articles and share them with others as long as they credit the authors and the publisher, but without permission to change them in any way or use them commercially.
A 78-year-old woman with a suspicious ischemic heart disease was referred to our clinic because significant myocardial ischemia at the left circumflex artery (LCx) on myocardial perfusion single-photon emission computed tomography with 317 calcium score on cardiac computed tomography was observed. Coronary angiography was performed via left snuffbox approach and it demonstrated intermediate to severe stenosis with focal heavily calcification in the LCx (Fig. 1A). Therefore, the plan was to perform optical coherence tomography (OCT)-guided percutaneous coronary intervention using rotational atherectomy for the LCx lesion using a 7.5 French sheathless guiding catheter (Eaucath, Asahi Intecc, Nagoya, Japan) via the left snuffbox approach. Following successful atherectomy with 1.25 mm and 1.50 mm burr size, post-atherectomy OCT demonstrated large calcium angle and thickness and a minimal lumen area of 1.22 mm2 in the LCx lesion (Fig. 1B–E; Suppl. Video 1). Circumferential and thick calcified plaque led to predilation with a 2.5 mm scoring balloon and then a 3.25 × 33 mm everolimus-eluting stent (Xeince Sierra®, Abbot Vascular, Santa Clara, CA, USA) was implanted. After post dilation with a 3.25 × 12 mm non-compliant balloon at up to 20 atm, post-stenting OCT and co-registration of OCT and coronary angiography demonstrated good stent apposition and a minimal stent area of 5.39 mm2 at the severe calcified area without stent edge dissection (Fig. 1F–J; Suppl. Video 2).
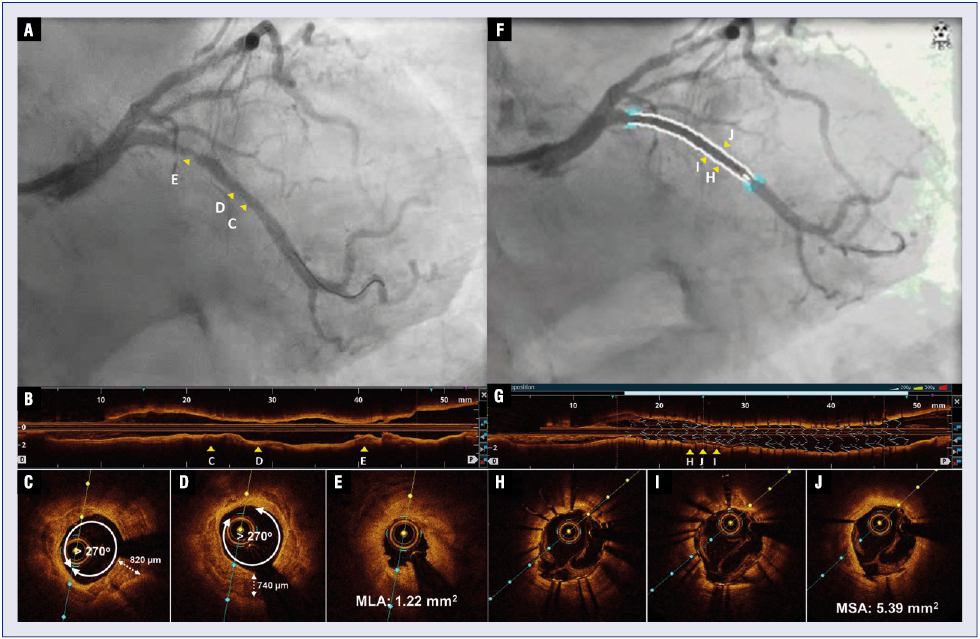
Figure 1. A. Post-atherectomy angiography showing the stenosis along the proximal left circumflex artery (LCx); B. A longitudinal optical coherence tomography (OCT) image; C, D. Cross-sectional OCT images showing severely circumferential calcified plaque with 820-μm and 740-μm thick layer; E. OCT showing the minimal lumen area (MLA) of 1.22 mm2; F. Simultaneous angiography and OCT co-registration image demonstrating no malaposition in stent implantation area.; G. Three-dimensional stent rendering image demonstrating successful proximal optimization technique without stent malposition supported by stent apposition index (sky-blue colored bar above OCT image); H, I. Cross-sectional OCT images demonstrating successfully expanded stent in severely calcified plaque; J. OCT showing the minimal stent area (MSA) of 5.39 mm2. The positions in longitudinal direction of C, D, and E are shown in A and B as yellow arrowheads. The positions in the longitudinal direction of H, I, and J were shown in F and G as yellow arrowheads.
This report highlights the benefit of OCT, which can penetrate calcium to visualize calcium thickness and have the superior resolution to confirm stent optimization in severe calcified lesions.



