Basic HTML Version
38
Acta Angiol, 2012, Vol. 18, No. 1
www.angiologia.pl
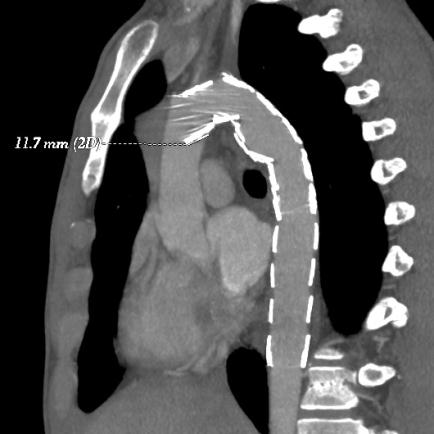
Figure 6.
One year later, follow-up CT-angiography showed no
endoleaks. The length of the lip of the endograft was observed
as 11 mm
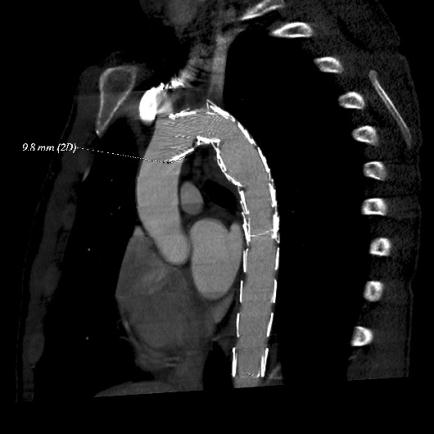
Figure 5.
Aortography after reimplantation of another
endograft (Zenith TX2 - Z-Trak-Puls). No endoleak was noted
Discussion
A patient suffering multiple trauma with thoracic
blunt aortic injury is very challenging for any medical
centre dealing with these kinds of traumas. It is worth
mentioning that a patient with a minor injury of the
thoracic aorta could be
treated in a conservative way
(an aggressive anti-impulsive treatment). This is espe-
cially important in young patients and maybe the best
solution would be to avoid endograft employment into
the thoracic aorta [6]. At the moment we can only
speculate about the possible changes in the wall of the
thoracic aorta and about the long-term behaviour of the
endograft (under consisted pulsative movements and
blood pressure forces).
Meanwhile, open surgery might include considerably
high risk in the case of multiple trauma patients. Blunt
trauma (especially after traffic accidents) consists of
significant forces frequently associated with injuries such
as traumatic brain injuries, (intra) abdominal injuries,
pulmonary contusions, long-bone fractures, etc. When
thoracotomy, thoracic aortic clamping (with or without
left-heart bypass), and attendant haemodynamic and co-
agulation fluctuations are added, the population’s perio-
perative management becomes even more challenging.
Under these circumstances, the intraluminal placement
of an endograft for these patients as mini-invasive treat-
ment seems to be the optimal clinical solution.
Considerations about the clinical decisions with re-
gard to the employment of the stent graft should be
based on thorough calculations with high-quality CT-
-angiography. Dynamic CT-angiography has shown the
difference of the diameter of the thoracic aorta to be
as much as 18% between the systol and the diastole,
and, additionally, the diameter of the thoracic aorta is
smaller in haemodynamically unstable patients [7]. This
could lead to the mismatching of diameters between
a real diameter of the thoracic aorta and the endo-
prosthesis. Thus, undersizing an endograft could cause
insecure fixation and sealing.
Conversely, an excessive oversizing may result in at-
tachment site endoleak, device infolding, collapse, and even
death fromaortic occlusion [8]. The “bird beak” deformity
as a phenomenon of endografting has been described after
employment of endografts. This sign characterizes the
proximal lip of an endograft that is not placed against the
inner wall of the thoracic aorta
[9] (Figure 3).
In our case, we used the
second generation of TAG
device, which, unfortunately, has been frequently as-
sociated with endograft collapse. In fact the smallest
diameter of GORE TAG (II generation) was 26 mm
and it was indicated for use in aortas with an inner wall
diameter of 23–24 mm (according to instructions). The
diameter of the thoracic aorta of 19–20 mm as in our
case could lead to a mismatch between the endograft
and the aortic wall. Muhs et al. (2007) showed that no
collapse of the second generation devices occurred in
patients treated with aortic diameters of
≤
23 mm [4].
One issue is a small diameter of the aorta, but should
it be combined with a small radius of curvature of the
aortic arch the most challenging anatomical situation
would lead to the collapse of endograft [10]. We would
like to emphasize that the Gore TAG device was chosen

